What Is Sepsis?
Signs Can Be Subtle, but the Consequences Can Be Dire
One September morning in 1928, Dr. Alexander Fleming returned to his lab after a family holiday to find colonies of mold invading his meticulously prepared Petri dishes. He had been studying the properties of staphylococci, a type of bacteria responsible for skin infections. The mold — specifically Penicillium — had killed all the bacteria on the dish surrounding it. His discovery led to the first antibiotic and humanity’s first tool to combat sepsis.
You may not have heard the word “sepsis” before, but you almost certainly know someone who has had it. Sepsis is the body’s dysfunctional reaction to a foreign invader — be that a staph infection, the flu, or COVID. What starts as the immune system’s attempt to fight the infection spirals out of control and leads to severe organ dysfunction. The end result may be confusion, kidney or liver failure, or shock, a life-threatening condition in which the body fails to maintain a safe blood pressure. If you have ever been hospitalized for an infection you likely had some form of sepsis.

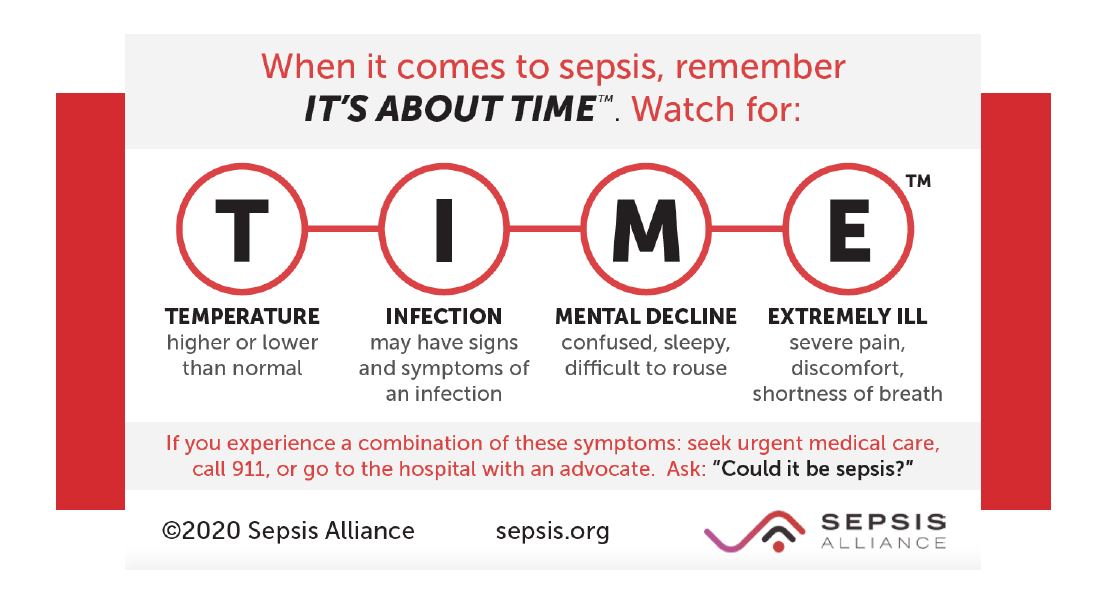
Most people recognize classic signs of a heart attack or stroke and know to seek help, but what about sepsis? It doesn’t cause crushing chest pain or facial droop, but can make a person feel “not quite right.” Maybe you had a little bit of a cough or a urinary tract infection, or you cut your foot at the beach. Maybe you didn’t realize your loved one was sick at all, but they just seem more tired and a little bit confused. The signs and symptoms are subtle and can be extremely difficult to recognize. If it isn’t identified and treated early enough, the consequences can be dire.
In the century since Dr. Fleming’s happy accident, we have made huge strides in the recognition and management of sepsis. Nevertheless, it remains a deadly and poorly understood disease. Over 1.5 million adults in the U.S. will experience sepsis this year, and over 350,000 of those will die. Sepsis is especially dangerous in children, older adults, and those with weakened immune systems. Some sepsis survivors face long recoveries, and may experience long-term effects such as decreased physical or cognitive function or post-traumatic stress.
The best thing you can do about sepsis is to learn more about it. Take measures to protect yourself and your family. Wash your hands, clean common surface areas, and get vaccinated against infections like influenza and COVID. Recognize the symptoms: fevers, weakness, shortness of breath, rapid heartbeat, chills, fatigue, or confusion, especially in someone with recent signs of infection. Most importantly, seek medical attention early — don’t wait until these symptoms become severe to get help.
Health-care providers are making constant efforts to improve our care of sepsis patients. This work is happening in your community; over a decade ago Cottage Health appointed a dedicated multi-disciplinary committee that develops protocols to identify and treat patients with sepsis as quickly as possible. As a result, sepsis survival rates at Cottage are well above the national average. Yet our work is not done; we remain committed to finding new ways to combat sepsis. This includes spreading the word on how to recognize signs of sepsis to our community and improve early detection and treatment.
September is Sepsis Awareness Month! Take this opportunity to talk to your loved ones about sepsis. If you are a sepsis survivor, consider sharing your story with others. Know that you are not alone. Together we can win the fight against sepsis.
Click here for more information about sepsis from Cottage Health.
You can also learn more about Sepsis Awareness Month from the Sepsis Alliance.
Dr. Natalie Achamallah is director of Critical Care Education and the Sepsis Multidisciplinary Committee at Santa Barbara Cottage Hospital.




You must be logged in to post a comment.