Four biology researchers at UC Santa Barbara have developed a CRISPR-associated protein that can be used to identify the presence of SARS-CoV-2, the virus that causes COVID-19. Their paper on their invention, in preprint at bioRxiv.org, brims with innovation and states their new CREST test is “low cost, highly sensitive, and easy to deploy at sites with minimal infrastructure.”
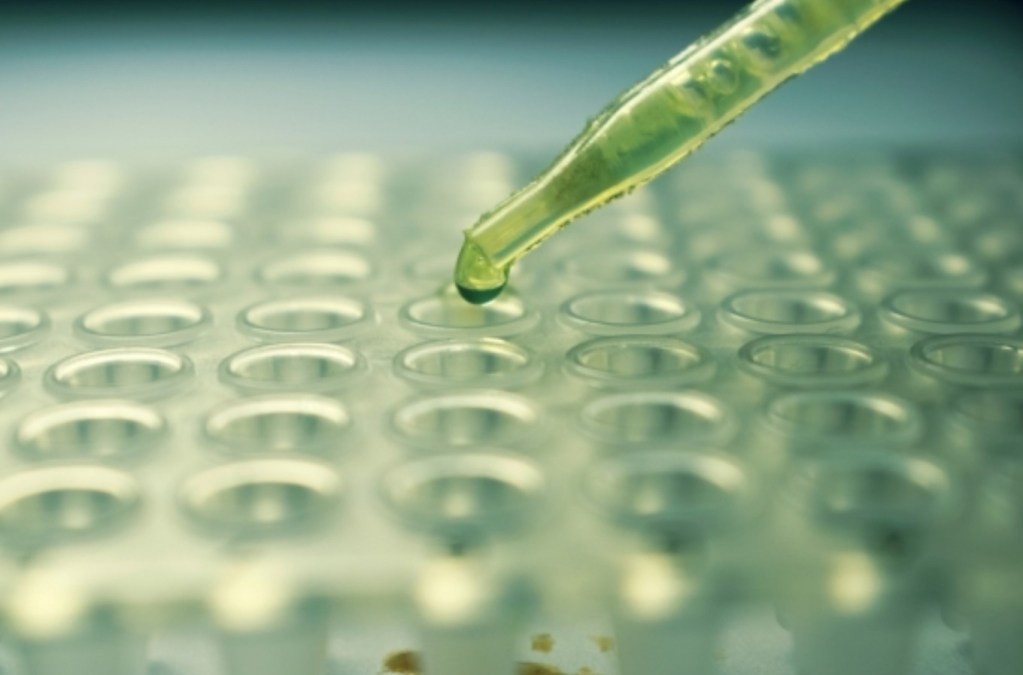
CREST — which stands for Cas13-based, Rugged, Equitable, Scalable Testing — can be done in the field and uses a DIY-inspired heating machine as part of the process. The protein created by Max Wilson, Carolina Arias, Diego Acosta-Alvear, and Kenneth Kosik was edited using CRISPR technology to recognize SARS-CoV2. As the virus invades, Cas13 starts “chewing” on it, Wilson explained. The RNA destruction causes fluorescent indicators to glow in the researchers’ assay immediately. “Our little wells just light up if the virus is present when we mix all these things together,” he said.
The current gold standard for COVID virus detection, the polymerase chain reaction (PCR) test, takes the virus’s RNA, builds the other half into a DNA strand, and duplicates it. Detection involves locating certain points on the strands, but the process requires a proprietary reagent produced in small batches, the paper explains. The limitation has caused delays in the widespread testing needed against the pandemic. The CREST test is “equivalent in sensitivity” to that test.
The Cas13 proteins are widely available, and the team purified enough protein for 500,000 tests from one liter of bacterial culture. Another advantage of the new CREST method is its cost: $5.90 per test compared to the PCR flow strip test cost of $14 apiece.
Tempering the excitement over the discovery is government regulation. A research lab like Wilson’s cannot cross over into studies involving humans, or a clinical trial, without permission. They would further need FDA approval for distribution of their new test, a years-long process currently shortened by Emergency Use Authorizations given for many COVID tests. They’re evaluating these hurdles, Wilson said, but not sitting still. The group is planning a surveillance study to sample asymptomatic people for infection. This would gain data, such as genetic changes in the virus, that could inform a response.
The four, who donated enough reagent to Cottage Health in early April to do 600 tests, came together from a variety of fields: Kosik’s work involves the brain, Acosta-Alvear’s cell stress response, Wilson’s cell perception, and Arias’s virus-host interactions. “I’ve been completely astounded by the level of coordination and innovation from my colleagues who just a few weeks ago were studying totally different things,” Wilson said.
A head-to-head comparison of the CREST test to the Centers for Disease Control and Prevention’s gold-standard PCR test is the team’s next step in their simple, low-cost test for the world.
[Update] After this story was posted, the Indy learned that the team is considering releasing the test in an open source format and also that CREST was 100 percent accurate in identifying the COVID virus.
At the Santa Barbara Independent, our staff continues to cover every aspect of the COVID-19 pandemic. Support the important work we do by making a direct contribution.